The healthcare industry is incredibly complex, often requiring heavily customized software to manage its intricacies. This complexity arises from legacy systems, highly regulated data, and inefficiencies across units, departments, organizations, and systems. These issues are further compounded by mergers, acquisitions, and the emergence of alternative care models, which demand interoperable solutions.
Off-the-shelf software, including artificial intelligence (AI) solutions, frequently falls short due to the need for significant modifications. As a result, custom healthcare software products present a viable alternative to optimize return on investment (ROI) in niche or complex situations.
In this guide, we will cover:
- What healthcare software product development entails
- Key healthcare software projects
- The development process, including challenges and regulatory considerations
- A comparison between in-house and outsourced development
What is Healthcare Software Product Development?
Healthcare software development involves creating custom software products (apps, embedded systems, business systems, platforms) for the healthcare industry—healthcare facilities, practitioners, payers, medical equipment manufacturers, pharmaceuticals, and their end users (e.g. patients).
Healthcare software can be used internally by the organization to automate processes, surface valuable insight, and simplify work. Healthcare software products can also be used externally by patients and other end users, including telehealth apps, wayfinding apps, and remote health monitoring.
What Is the Current State of the Healthcare Software Development Market?
As a highly regulated and complex industry with many stakeholders, the software used in healthcare is often highly customized. All healthcare software must reflect a deep understanding of the healthcare system and its unique needs, constraints, and legal requirements.
According to the latest research from Dimension Market Research, the healthcare software-as-a-service (SaaS) market is set to reach $93.4 billion by 2033, up from $36.8 billion in 2024.
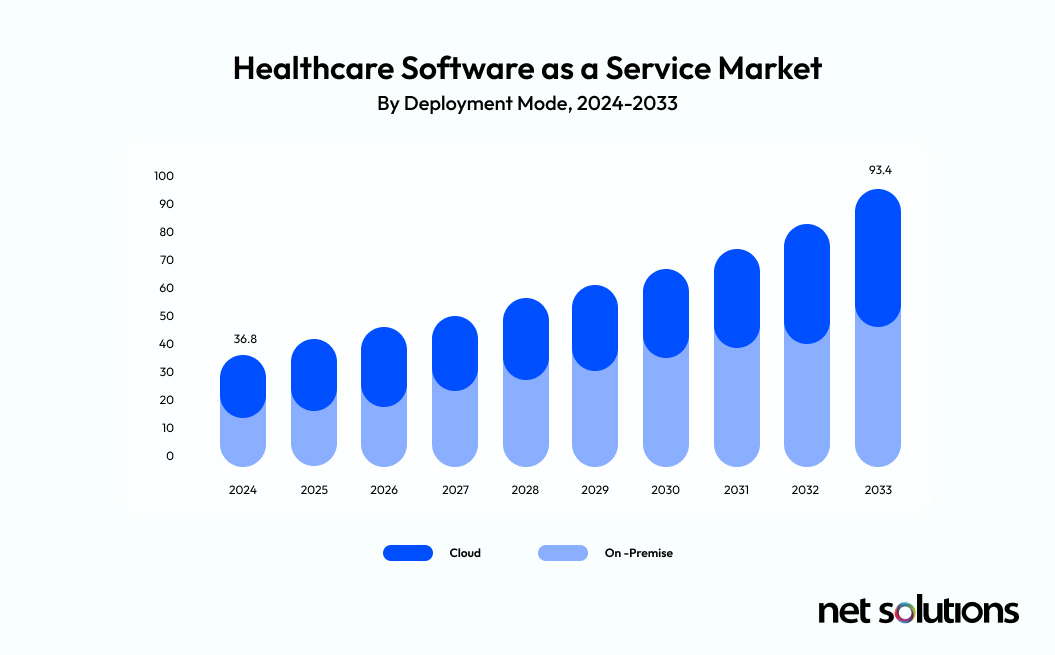
Healthcare organizations are undergoing their own digital transformations, relying on a greater use of the cloud and SaaS products (both off-the-shelf and bespoke) to improve operational efficiency (cost benefits), meet security requirements, and deliver better patient care.
A growing number of solutions are now also leveraging artificial intelligence (AI) and machine learning to make sense of big data and surface critical insights that can further improve administrative processes and patient outcomes.
What Are the Different Types of Healthcare Software Systems?
Healthcare software includes a wide range of products that are used in-house or in the cloud (SaaS) to support healthcare operations or patient care. Some primary examples include:
Electronic Health/Medical Records (EHR/EMR)
Systems designed to manage patient medical records, created based on interactions with clinicians or administrators. These databases include a range of data, including personal details, demographics, medical history, medication, immunization status, lab and imaging results, and more.
Telemedicine / Telehealth Platforms
Software that supports two-way synchronous or asynchronous communication between clinicians (physicians, nurses) and patients. Communication can include email, chat, video, or phone. In addition, platforms may include components on education/intervention, reminders, and remote monitoring. While used interchangeably, telehealth includes preventative care, whereas telemedicine is narrowed to diagnosis and monitoring.
Practice Management Systems (PMS)
Software used in healthcare practices to manage the financial and administrative details associated with the office. Some PMS systems include patient access to medical records and appointment management features.
Revenue Cycle Management (RCM) Solutions / Medical Billing Software
Software specifically designed to support the revenue cycle, including prior-authorization and eligibility verification, billing, coding, and auditing. Most feature analytics (predictive and retroactive) and help identify process improvements. It may include advanced capabilities to manage patient payments and co-pay.
Patient Portals / Patient Communication / Appointment Booking
Independently or as part of other solutions, patient-facing solutions such as all-in-one portals or independent tools (communication, appointment management) support digital access to personal health information and streamlined interactions (intake forms, access to records, automated reminders).
Payer Systems
A variety of systems used by payers (insurers) to manage healthcare claims and payments, including coding and billing reviews, prior authorizations, auditing, and contracting.
Laboratory Information Systems (LIS)
Systems used by healthcare labs to support lab operations, including logging and tracking samples, processing samples, recording data, and compiling that data into reports.
Remote Patient Monitoring (RPM)
Software designed to help monitor patients outside of clinical settings. This can include self-reported information (e.g., blood pressure, weight) or the use of technology/mobile devices to capture and report data automatically. It is considered a part of telehealth or mHealth.
Mobile Health / Health Tracking Apps (mHealth)
Apps used to support care delivery, either in the clinical or patient setting. mHealth apps can include access to clinical research, diagnostic or treatment support, training, remote monitoring, and tools used by patients, including education, treatment support, or preventative outreach. Patients may also independently download health tracking apps to self-monitor their health.
Clinical Communication and Collaboration
Support clinical workflows and collaboration with a secure solution that accurately routes information to the correct team member(s) and escalates critical communication following defined paths. It may include capabilities for call management, patient messaging, or telehealth.
ePrescribing
Highly regulated software to support secure digital creation and transmission of prescriptions to a pharmacy.
Staff Management / Staffing
Human resource management (HRM) systems to manage scheduling and staffing in complex healthcare situations. Includes specialized software to manage shift work, agency coordination, and staffing level calculations to support quality of care and budget goals.
How to Develop a Healthcare Software Product
As with any software product, the key to success begins at the planning phase where you visualize the problem you’re trying to solve and how to efficiently and securely solve that problem. The following are steps you would take in your development process.
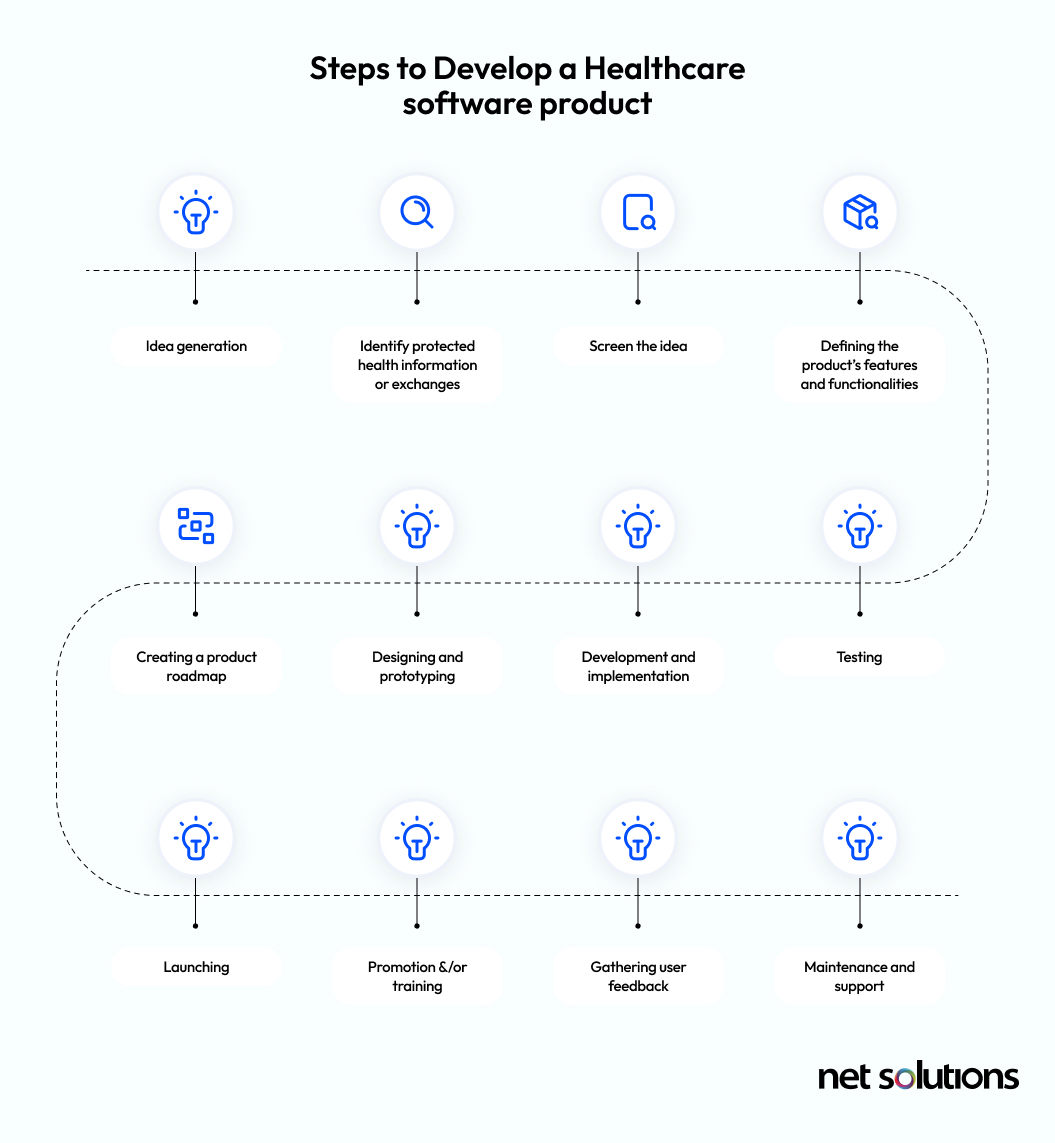
Idea Generation
Work with relevant stakeholders to identify the problem (in human-centric terms) and look for solutions to the problem. If none exists, what gaps are present (integration, security, functionality) that could help you come up with possible solutions?
Identify Protected Health Information or Exchanges
Identify if the app deals with protected health information or health information exchanges, which will subject it to a higher level of regulatory oversight.
Screen the Idea
Review the available solutions with relevant stakeholders and ideally those with the technical knowledge for execution (internal developers or external partners), to ensure the idea is feasible.
Defining the Product’s Features and Functionalities
Build out a detailed version of the idea, which can be used to define the features and functionalities of the product.
Creating a Product Roadmap
Gather all available features into a product backlog, determine which features should be prioritized for the minimum viable product (MVP), and create a roadmap to meet short and long-term goals.
Designing and Prototyping
Create wireframes and prototypes to test the idea, including getting user feedback on the user interface (UI) and user experience (UX), as well as conducting preliminary compliance and security checks. Ensure the target users are willing to use the solution and that the product effectively solves the identified problem.
Development and Implementation
Develop the product. If following Agile for the product development, proceed toward an MVP that focuses on incremental and iterative development cycles, including regular feedback loops.
Testing
While testing is included in the Agile process, it is critical that the MVP of a healthcare product undergo rigorous testing to ensure it meets security, privacy, and compliance requirements. For US-based products, software developers should follow a HIPAA-compliant testing process.
Launching
Launch the product with a “build, measure, learn” mindset to ensure continuous improvement. If clinicians are the end users—who are often resistant to change—begin with a small alpha group to gather feedback before implementing changes to clinical workflows.
Promotion and Training
If the product is to be used by a large group of internal or external users, a strong marketing and promotion strategy is essential to highlight its benefits. For internal solutions requiring changes in clinical workflows, training programs, an incremental rollout plan, and support from champions at the executive, department, or unit level will be necessary.
Gathering User Feedback
As technology and user expectations evolve, it is crucial to gather continuous feedback to keep the product relevant. The product backlog should be refined regularly, and improvements should be reprioritized based on user input.
Maintenance and Support
Healthcare software requires ongoing maintenance and support to meet shifting compliance requirements and to ensure seamless integration with evolving healthcare technology infrastructures. Many new regulations now focus on securing the software supply chain, necessitating a greater vetting of third-party code and libraries and the implementation of secure code-signing processes.
To learn more, we have put together a product development checklist that may be helpful.
What Are the Challenges of Healthcare Software Product Development?
There are a number of challenges unique to healthcare that can make software product development difficult. These challenges stem from regulatory requirements, interoperability concerns, and resistance to change, among other factors.
1. Regulatory Considerations
Healthcare software must be designed with appropriate technical and organizational measures (TOMs) to ensure the security and privacy of data while meeting complex regulatory requirements. These may include cloud security standards, medical device regulations, and national compliance laws.
2. Interoperability
Healthcare software often needs to support health information exchanges (HIE), which require compliance with standards such as HL7 and FHIR to ensure seamless data sharing across different systems.
3. Tech Stack Selection
Choosing the right technology is key to ensuring the solution works within the overall healthcare infrastructure and is future-proof to evolving needs and technologies impacting the future of software development (e.g. considers scalability, integration with AI)
4. Operational Limitations
Some healthcare software solutions are mission-critical, meaning they require high availability and robust protections to ensure uptime. In cases where constant connectivity is not possible, offline functionality may be necessary.
5. Resistance to Change
Clinicians and healthcare staff are often resistant to changes in workflow, as they prioritize accuracy and efficiency in patient care. To ensure successful adoption, products must be developed with input from stakeholders and introduced gradually.
6. Time to Market
Decision-making in large healthcare organizations is often slow, resulting in prolonged development cycles. This delay can cause a misalignment between the identified problem and the solution by the time the project is approved.
What Are the Standards and Regulations for Healthcare Software Product Development?
All healthcare software is subject to regulatory oversight, but some solutions require even more stringent measures. Regulations are constantly evolving, making it critical to stay updated on requirements at the global, federal, state, and industry levels.

Key Regulations in Healthcare Software Development
Some examples of important healthcare regulations include, but are not limited to:
- GDPR, PIPEDA, FTC Act, and state laws governing strong data security practices.
- HIPAA, which requires physical, technical, and administrative safeguards for healthcare data protection.
- HITECH, which incentivizes the use of EHRs and strengthens security requirements.
- FDA CFR 21 Part 11, EPCS, and eIDAS, which set standards on electronic signatures for prescribing and documentation.
- CURES Act Final Rule, which defines security for the exchange of electronic health information.
- NSM-22, which establishes new risk management requirements for US healthcare organizations.
- NIS-2, which sets new risk management requirements in the EU, including Zero Trust security measures.
- EU Cybersecurity Act, which establishes requirements for all information and communications technology (ICT) products.
For some US healthcare organizations, additional considerations may apply when entering contracts or partnerships with government entities, such as compliance with Executive Order 14028 (EO 14028).
Healthcare Standards and Certifications
A number of healthcare standards and frameworks have evolved to support best practices and/or to meet the requirements for specific regulations. Bodies such as the ISO, NIST, ENISA, the FDA, and the Medical Device Directive (MDD) and Medical Device Regulation (MDR) in the EU and UK should be referenced, depending on the specific type of product being developed. Healthcare entities may require proof of certifications (e.g. ISO 27001, HITRUST).
Emerging Technologies in Healthcare Software Development
There are many critical decisions to make in choosing the technologies that will make up your healthcare product, some of which may be constrained by existing systems. The choice of technology is driven by the project requirements, regulatory requirements, desired features, and specific goals around cloud, scalability, performance, or other factors. Team expertise may play into these decisions, but should not be a limiting factor. Consider how external software development experts can supplement or support your team.
The following technology trends are currently influencing healthcare software development:
Artificial Intelligence (AI) and Machine Learning (ML)
Healthcare is increasingly “AI-enabled,” both within the clinical context and for patient-facing products. Data science (machine learning) and AI are being used to:
- Generate real-world evidence (RWE) from clinical data to support clinical decision making (e.g. identify potential anomalies from data or imaging).
- Support patient queries (e.g. symptom checker chatbots) and workflows (e.g. patient recall).
- Automate workflows (e.g. intelligent coding).
- Support health monitoring.
- Greater real-time capabilities (e.g. alerts).
- Make autonomous payment decisions (e.g. insurer approvals).
Blockchain
The potential for blockchain to record and share data could help healthcare organizations and systems become more interoperable and support patient outcomes.
Wearables and Apps
Wearables and mHealth apps are increasingly being trusted to assist clinicians with tracking patient compliance to healthcare plans and in preventative medicine.
Robotics
Robotics are combined with intelligent software to support precision healthcare, automate repetitive tasks (e.g. pharmaceutical dispensing) and assist clinical specialists with complex situations (even operations).
Virtual Reality (VR) and Augmented Reality (AR)
VR and AR are being used creatively to simulate training, to visualize medical issues for patients, or to support medical device development.
What Are the Costs of Healthcare Software Product Development?
The cost of software development will vary from product to product, depending on several factors:
- The type of product being created (e.g. mobile app, EHR), with software dealing with personal health information significantly more costly than an internal app designed to improve workflow.
- The complexity of the project (the number of features or workflows in the product backlog, the complexity of features, how much is proprietary vs library-based).
- Hiring models (in-house, outsourcing).
- The scope of the project, including costs for strategy, market research, product design, user experience testing, development, and QA testing.
- The complexity of security requirements.
- The cost of infrastructure or third-party tools.
Healthcare Software Product Development: In-House Team or Outsourcing?
When what you want is not available as an off-the-shelf solution, or when relying on a vendor’s product development timeline no longer suits you, you can develop your own healthcare product. However, having an in-house solution does not always mean relying on in-house developers.
In the below table, we will explore the considerations for in-house development vs outsourced product development to a local agency or offshore (out-of-country) development partner.
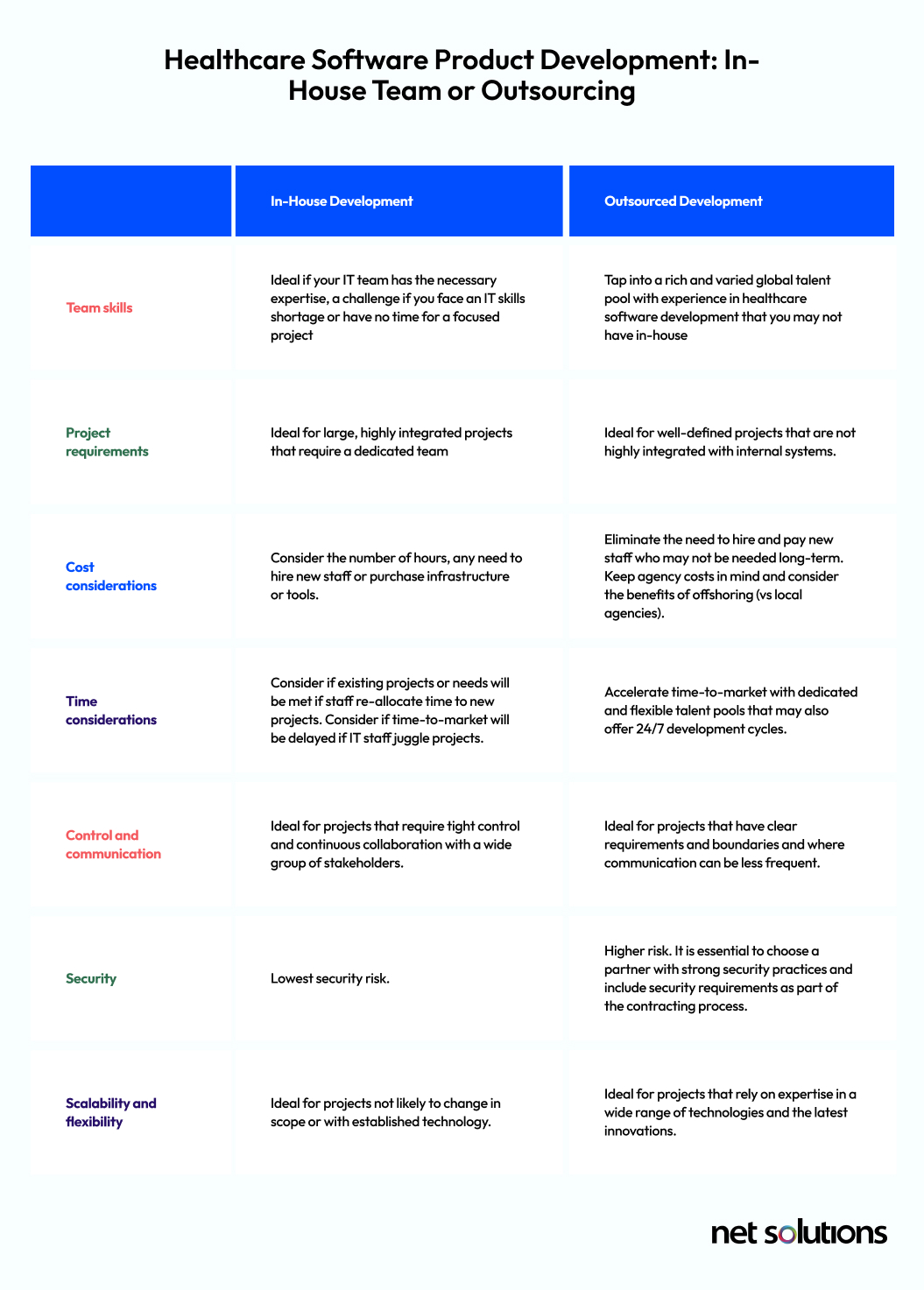
In-House Software Product Development
Using existing or newly-hired IT staff provides the greatest amount of control over the software development process and intellectual property.
- Business expertise: In-house developers have first-hand knowledge about your internal systems and processes, the challenges you face, and overarching business needs.
- System expertise: In-house developers are familiar with your tech stack and understand the complexities of fitting new software into the ecosystem.
- Collaboration: In-house developers have ready access to stakeholders to create and refine the product backlog during the development process, with a great deal of trust to encourage collaboration. Direct face-to-face communication can be essential when facing complex problems and avoiding misunderstandings that could result in product misalignment.
- Cultural fit: In-house developers align with the company and are motivated to support the business goals.
Despite these benefits, many healthcare organizations find that in-house development is simply not realistic, due to:
- Smaller IT teams may result in a lack of appropriate skills and lack of knowledge of emerging technology.
- Smaller IT teams may not have extensive experience building software from the ground up.
- The long and costly process of hiring (and retaining) staff to gain access to skills.
- Competing priorities that interrupt the development process, reducing time-to-market.
- The high cost of staff hours vs outsourced services.
Outsourced Software Product Development
While in-house development is appropriate for many projects, the strategic decision to outsource can help healthcare organizations realize significant benefits, including:
- Global talent pool: Access a global talent pool with varied and deep knowledge of specific and emerging technologies in software development. As experts in software development, agencies continue to invest in upskilling their employees to meet the demands of the market. Add or remove specific individuals to projects as needed, all bundled into the cost of development.
- Cost effective: Outsourcing has the potential to save money versus hiring in-house staff, although outsourcing to local agencies can come with a high price tag. Offshore agencies experience lower wages and lower overhead and can leverage deep expertise to develop at a faster pace, savings they can pass along to you.
- Faster time to market: Access a scalable talent pool that is staggered across locations to increase the speed of development or that has dedicated developers working on your project without getting pulled into other projects or situations.
There are many factors to consider when looking at outsourced development. We encourage you to read more in our guide to offshore development.
How to Choose the Right Healthcare Software Product Development Partner
Finding a development partner with the knowledge of the challenges within healthcare, a nuanced understanding of security requirements, and the experience building compliant solutions can be challenging. It is critical to carefully vet potential partners to ensure you not only receive the optimal solution for your challenges, but that development complies with requirements for business associates.
Here are a few factors you could consider:
- Technology experience: The ideal development partner will have deep technical expertise, including the latest technologies (e.g. artificial intelligence, analytics, passkeys) and specific expertise that may be relevant to your needs such as FHIR, DICOM, or HL7. If you are in the EU, you’ll also want to look for a partner who is exploring emerging requirements for digital wallets, which will soon govern identity and access to online health services.
- Success stories: Consider development partners who have experience specifically within healthcare. Read case studies or ask for references.
- Human-centric design and development processes: Look for a partner who takes a human-centric approach to strategy, user experience (UX) design and development, leveraging Agile processes to iterate development with cycles of feedback and user testing.
- Accreditation: Look for partners who have security certifications, demonstrating appropriate controls and processes for software development and/or cloud security, e.g. ISO 27001 or HITRUST certification.
- Information risk management processes: In order to protect intellectual property (IP), look for partners with well-defined risk management processes, with details on access controls and authentication, secure code signing, encryption, defense systems, logging, and incident management processes.
Ready to Start Your Healthcare Software Product Development Project?
If you are ready to transform your healthcare business with a bespoke software solution, it is critical to choose a partner with a global record of developing highly technical projects that meet strict security and performance requirements.
For more than 20 years, Net Solutions has been building custom healthcare solutions including patient portals, remote patient monitoring apps, telemedicine solutions, and medical practice software. Net Solutions is ISO/IEC 27001 certified.